A time to heal
India’s tribal communities deserve far better than what the country’s healthcare system and its policymaking have delivered thus far
The Constitution of India recognises the special status of tribal communities — the scheduled tribes, as they are called — and provides safeguards to protect their rights and culture. There are 705 tribes, about 104 million tribals in total (8.6% of the country’s population) and they are located in 10 states and in the Northeastern region.
The numbers are sizeable and these are our fellow-citizens, but India’s tribespeople have remained on the margins — geographically, socioeconomically, politically and in the national psyche. From the mainstream perspective, tribals are “those semi-naked wild people who live somewhere in the forests and mountains, and who sometimes appear in the news because their children are malnourished”. Such views damage the tribal cause.
Dr Abhay Bang is a physician and public health researcher who works in the largely tribal district of Gadchiroli in Maharashtra
Though it has long been suspected that tribals have poor health indicators and unmet needs, healthcare for them has been neglected. The terrain and environment in which they tend to live, unique social systems, different cultural norms, diverse disease prevalence and higher mortality rates place tribals at a considerable disadvantage.
Not surprisingly, healthcare in tribal areas is an unsolved problem. But how would the nation know? No separate data on tribal health has been maintained and that has meant a blissful unawareness of the health of tribal people.
The Government of India recognised that it needed to view the health of tribespeople as a serious and special concern and that led to the formation, in 2013, of an expert committee constituted jointly by the Ministry of Health and Family Welfare and the Ministry of Tribal Affairs.
The task before the committee was to provide answers to two questions: what is the present status of health and healthcare in tribal areas and why the gap, and what should the roadmap for the future be to close this gap rapidly.
The expert committee’s report — Tribal Health in India: Bridging the Gap and Roadmap for the Future — reveals that tribal people suffered from a ‘triple burden of disease’. First, maternal and child health issues and communicable diseases; second, the rising burden of noncommunicable diseases such as hypertension and cancer; and third, mental health problems and addiction.
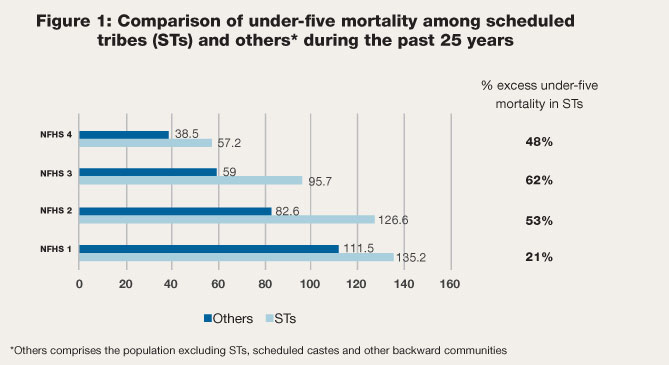
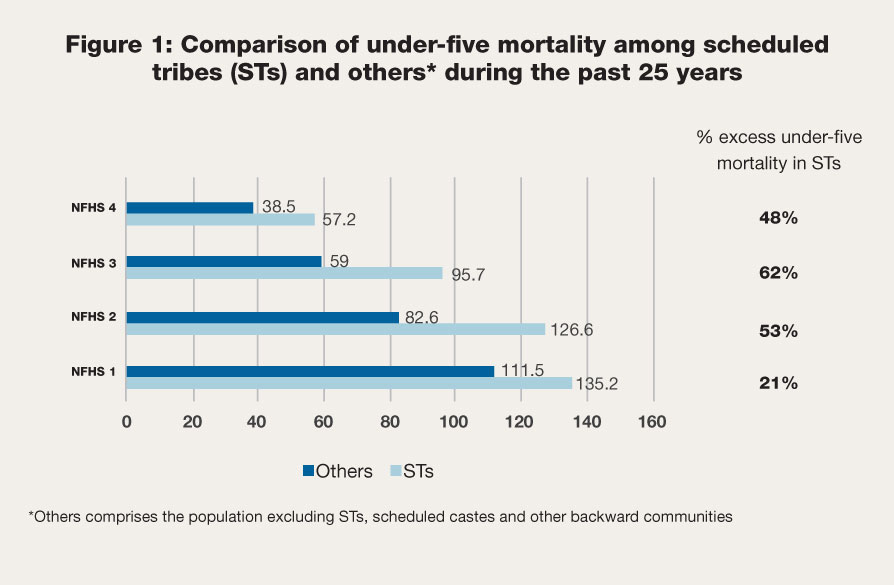
Though the health status of India’s tribals has improved significantly over the past 25 years, they are worse off when compared with other social groups. For example, child mortality in the under-five segment among tribal communities declined from 135 per 1,000 people in 1990 to 57 by 2015. But that’s still one-and-a-half times higher than that for the non-tribal population (figure 1).
Most malnourished
The percentage of underweight tribal children has come down from 54.5% in the National Family Health Survey (NFHS-3) conducted for 2005-06 to 42% in NFHS-4 (2015-16). But, compared with other social groups, tribal children continue to be the most malnourished.
The number of underweight tribal children is almost one-and-a-half times that of children in the ‘others’ category. Increased malnutrition and child deaths are reported time and again from tribal pockets across the country and the issue is discussed regularly in state legislatures. To little avail.
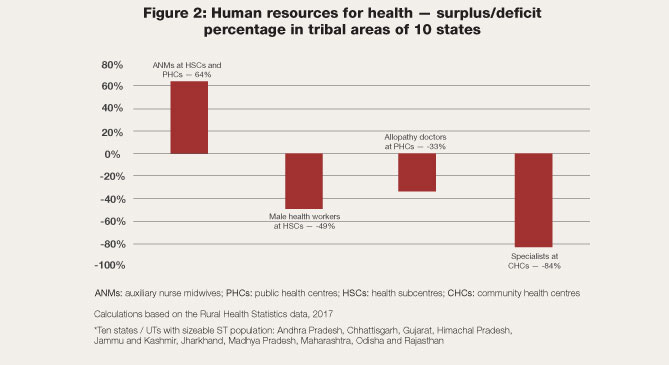
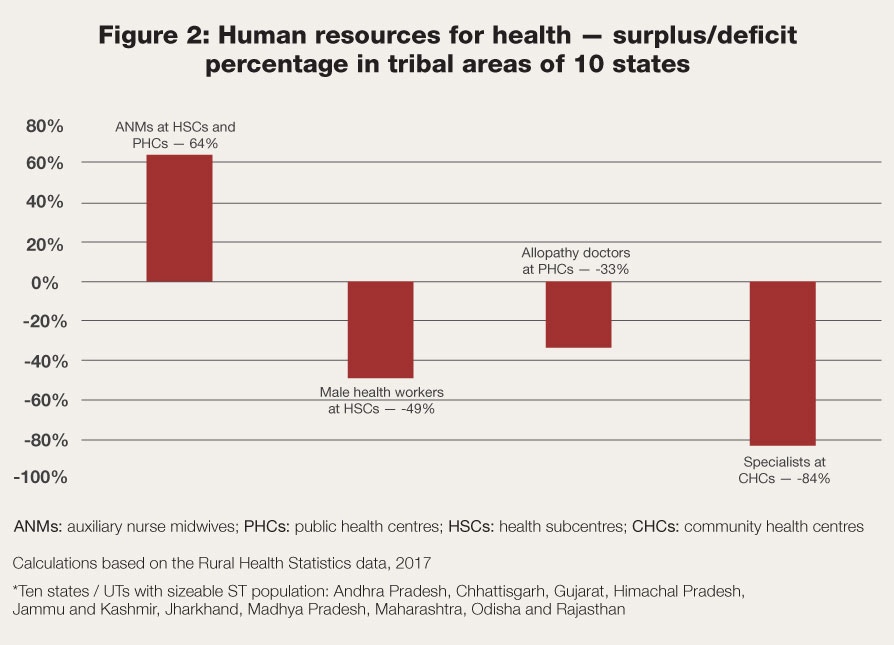
The tribal population carries nearly half of the burden of malaria in India and tuberculosis is three times more common among them. As the committee found, healthcare services in tribal areas, apart from being deficient in number, quality and resources, suffer from major design problems, mainly their inappropriateness to tribal society and lack of participation by the tribals themselves.
Dependent on public healthcare
Nearly 50% of outpatient visits by tribal people are to public health institutions and more than two-thirds of hospitalisation cases among them are in government facilities. The comparable proportions in the ‘others’ group are 18.5% and 34.5% respectively. This proves that tribal people, when they seek external healthcare, depend heavily on publicly funded ones.
What this signals is the need to strengthen public health facilities in tribal areas and to ensure that these are run by qualified and sensitive health functionaries, professionals who treat their patients with respect. Unfortunately, that is rarely the reality.
The expert committee report identified the principles of tribal healthcare and proposed an objective: that the health status of India’s tribals be brought on par with the rest of the population over the following 10 years.
With universal healthcare and universal health assurance being accepted tenets of government policy, the committee recommended that, in the spirit of the constitutional promise to the country’s tribal people, the implementation of these two should begin with the tribal population.
The roadmap suggested includes a healthcare delivery pattern and governance structure, and the necessary human and financial resources. The good news is that within the limits of the guidelines laid down in the National Health Policy (2016), it is possible to finance tribal healthcare, provided the central and state governments actually adhere to these guidelines. The question is if they will. That would be a test of India’s inclusiveness.