‘India doesn’t need more policies; it needs better implementation’
Arjan de Wagt makes a plateful of points about nutrition in India and they add up to plenty of food for thought about a crisis that continues to challenge the country. Despite the many positives here, the chief of nutrition with Unicef India sees “a disconnect between nutrition schemes and the nutrition status of women and children”.
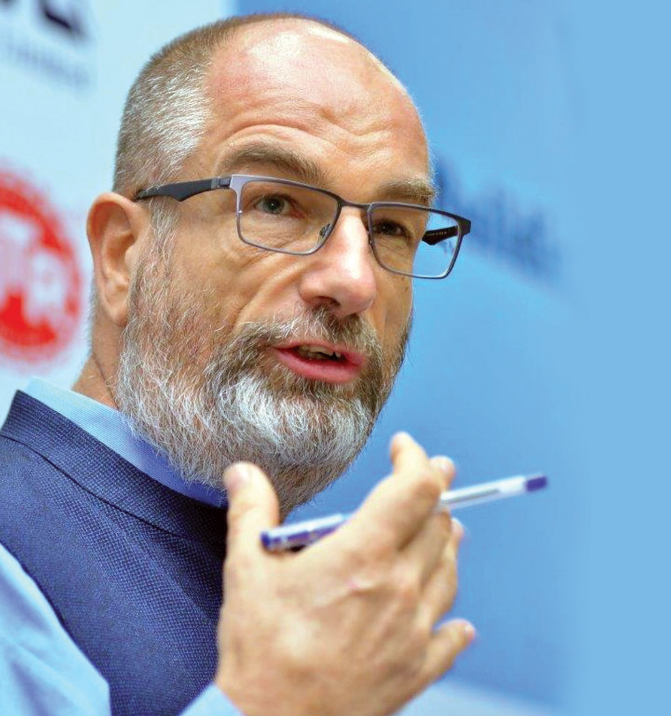
Mr de Wagt, a Dutch national who was previously with Unicef Nigeria, speaks to Labonita Ghosh about India’s nutrition challenges, how to best spend the resources that are available, and the necessity of creating awareness about adequate nourishment for mother and child. Excerpts from the interview:
What is the state of nutrition in India today? What are the challenges and what solutions have worked?
I have been a ‘nutrition visitor’ to India for five years and I’ve seen amazing policies and programmes here. There are many countries that don’t have anything like an Integrated Child Development Services system or 1.4 million anganwadis [childcare centres] and as many anganwadi workers. The quality of India’s nutrition guidelines and tools is high. Despite this, I see a disconnect between nutrition schemes and the nutrition status of women and children. Implementation has clearly been a challenge.
The percentage of children who receive vitamin A supplements and take-home rations and the percentage of pregnant women who receive cash transfers, deliver in hospitals and start breastfeeding in the first hour after childbirth are too low. As is the percentage of pregnant women, adolescent girls and young children who receive iron folic tablets to reduce anaemia. These interventions must have 70, 80, even 90% coverage to have the desired impact, which they don’t.
When coverage increases from 10% to, say, 50%, it usually includes those who are easy to reach rather than those who need help the most. Malnourished kids, for example, are typically found among those who are not easily reached by services. You must have good quality interventions reaching the most vulnerable, who often are also the most malnourished and usually the least likely to be able to access services.
Additionally, you need to address gender issues. Do women have enough time to care for children, or are they too busy with household tasks? Who makes decisions about the utilisation of financial and other resources in the household? If there’s healthy food, on whose plate does it end up?
Then there’s poverty as a major underlying cause of malnutrition. Some say that if you address poverty, you address malnutrition. But India’s National Health Surveys tell us that among the poorest 20% of households, 50% of the children are stunted. This also means that the other 50% are not stunted. In fact, there is 20% stunting among children in the richest households in India. Poverty doesn’t explain everything. You need the right services and a complete package to reach everyone. Why doesn’t that happen? Because delivery systems are often not strong enough.
As for financing, I think there’s substantial funding but not all of it is spent on evidence-informed, high-impact interventions. For instance, you need adequate numbers of well-trained human resources. Do we have enough frontline workers? Can we expect an anganwadi worker to do all the tasks she’s supposed to if financial support, supervision and guidance are not always there?
Why is on-ground implementation such a challenge in India?
In many cases people don’t know what healthy nutrition, diets and child feeding are. Yet we expect communities to be able to feed their children well. We have to recognise that the government cannot, by itself, stop malnutrition; eventually families and communities have to do their bit by availing the services on offer.
While Covid awareness was delivered through simple messages about safety and hygiene, nutrition is more complicated. It starts with what you do as a pregnant woman and when the child is born. When do you start breastfeeding? What if the child doesn’t want to suckle? It’s not easy. But who’s helping people understand all this?
The solution to malnutrition is to stick to what you were planning to do. India doesn’t need more policies; it needs better implementation and that requires going back to the fundamentals and repairing systems when they are broken. We need to invest more in creating awareness on nutrition and healthy eating — I call it ‘nutrition literacy’ — and community nutrition empowerment.

India’s health expenditure is barely 1.5% of its GDP. How much of a handicap is that in improving healthcare in the country?
Of course, we need more money but I think we need better results for the money that we have — not just more money for nutrition but also more nutrition for the money that is there. I wonder how we can better support not only policymakers at the district and ward levels but also families in making decisions about limited resources, and get the maximum nutrition impact from them.
I was excited when Poshan Abhiyaan was launched because there was a good attempt at strengthening systems through increased training of frontline workers, and by states and districts reviewing and upgrading their anganwadi centres and using resources that had been underutilised. I started to see districts and states push for more frontline workers, and all of this was within existing budgets.
I think we need better results for the money that we have — not just more money for nutrition but also more nutrition for the money that is there."
How can data and technology be employed to improve nutrition outcomes and healthcare in general?
Too often we say we want more evidence and more data. I would say we need more use out of the data we have. Are people looking at what is happening at the district, ward and even village level? Is that data being linked to interventions? The system will show if there’s a shortage of iron folic tablets or take-home rations. But if nobody is looking at that, and picking up the phone to do something about it, then you have a problem.
Technology provides the opportunity to make data more accessible and usable. But if the anganwadi worker, her supervisor or people in the ward don’t know what to do with such information, or if they are not empowered to act, or if there are no funds or vehicles to transport supplies to a village, then the data is not useful.
Which states have managed their healthcare and nutrition issues well and why? What about the laggards?
The International Food Policy Research Institute, NITI Aayog [the Indian government think tank], the World Bank and Unicef conducted an analysis of four states (Tamil Nadu, Odisha, Chhattisgarh and Gujarat) where there has been a reduction in stunting to see how this happened. Nutrition and health interventions reaching children contributed about one-fourth, while poverty reduction, gender, education, etc were also critical.
States that have made some progress typically have a comprehensive response, success in reaching the most vulnerable sections and good coverage, with a full package of multisectoral services, whether social protection, water and sanitation, health or nutrition. Their systems function better because of the energy, time, finances and leadership they have invested in them.

How advantageous are collaborations between government and civil society in the nutrition space?
If you mean civil society in a broader sense, there are advantages. In Poshan Abhiyaan, a lot of effort has gone into mobilising frontline workers and having them promote awareness around nutrition as a Jan Andolan [people’s movement]. There has been some investment in mass media, though I don’t think it’s enough.
Some years ago, on a road trip from Delhi to Madhya Pradesh, I came across a breastfeeding shelter. Outside the shelter there was some messaging about breastfeeding. But this was after I had seen hundreds of billboards advertising colas, instant noodles and other junk food. Over the 2,600 km that we travelled, the breastfeeding message was the only one about healthy nutrition.
At Unicef we are working with 220 companies to create impactful nutrition and mobilise the private sector. Imagine if there were 10,000 companies and each of them educated each of their employees about healthy nutrition. They could easily integrate this with their existing CSR [corporate social responsibility] mandate and also pass on the message to clients.
Civil society in general — from religious groups to even neighbourhoods and building societies — could talk about healthy nutrition. If they can spread the word about Covid safety protocols, why not nutrition? To me that’s the potential of civil society.
