‘Public’ is the key
The public health system in India has come a long way, but there remains plenty left to accomplish in providing quality medical care to all of the country’s citizens
As a country of more than 1.4 billion people, almost 17% of the world population, India has a big role to play in achieving global goals relating to health. The country is going through a transition stage in terms of epidemiology (from communicable to noncommunicable diseases), demography (an increasing elderly population) and economy (a widening gap between poor and rich). These transitions are the key barriers, apart from geographical and cultural disparities, in catering to the health needs of all Indians.

Sita Rama Budaraju is a senior advisor with the Tata Trusts health team
A particularly vital category that needs specific healthcare consideration is mothers, newborns and children. The news on this is skewed. The National Family Health Survey 5 (2019-21) shows better maternal, newborn and child healthcare services and outcomes in the southern states, an example of which is ensuring at least four antenatal care visits for pregnant women. This is the kind of attention that leads to better results in achieving the United Nations Sustainable Development Goals (SDGs) on reducing infant and maternal mortality.
The past few decades have seen substantial progress in terms of mother and child health indicators. The decline in infant and maternal mortality rates that India has recorded can be attributed to the comprehensive approach adopted on what is called RMNCH+A (reproductive, maternal, newborn, child and adolescent health), as well as various government initiatives.
When it comes to communicable diseases, government programmes have succeeded in eradicating polio, guinea worm disease and yaws. In spite of this, India still carries a high burden of tuberculosis and AIDS patients. With noncommunicable diseases, there is a high prevalence of anaemia, diabetes and hypertension in the country (in diabetes, surprisingly, the southern regions show a higher incidence than the central and northern states).

Satish V Khalikar is a programme manager with the Tata Trusts health team
Immediate challenges
Whether it be communicable and noncommunicable diseases or maternal and child wellbeing, there are many issues that dog the Indian healthcare system: low governmental spending on health, poor coordination between the public and private healthcare sectors — and even between the centre and the states in policy matters — unequal distribution of the health workforce, poor quality of services in government health centres and a weak referral system. These are the immediate challenges to be overcome to ensure enhanced healthcare outcomes and to get to the SDGs within the set timeframe.
There are other issues that have slowed India down in attaining universal and quality healthcare for its people. One such concerns the setting up of medical colleges. Policy-level barriers in establishing medical colleges has led to a severe shortage of doctors, resulting in an abysmal doctor-patient ratio (1:850, which is better than the World Health Organization standard of 1:1000 but still far from satisfactory). The need of the hour is to encourage the setting up of many more medical colleges.
Then there’s the neglect that plagues preventive healthcare. The new ‘health and wellness centres’ that are replacing the traditional primary healthcare centres will be helpful in shifting the paradigm from ‘illness to wellness’.
Another point that requires addressing is the failure in implementing basic infrastructure and equipment readiness at government health facilities as per standards cemented by policy. This adds to the shift of patients from government to private hospitals, which translates into out-of-pocket expenses that can bankrupt poor and middle-class folks.
There is a silver lining, as always, amid all the negatives. Newly introduced programmes like the Ayushman Bharat Digital Mission and the Pradhan Mantri Jan Arogya Yojana certainly have the potential to improve the availability, accessibility and affordability of healthcare if implemented in a patient-centric manner. That’s a huge if but it’s possible.
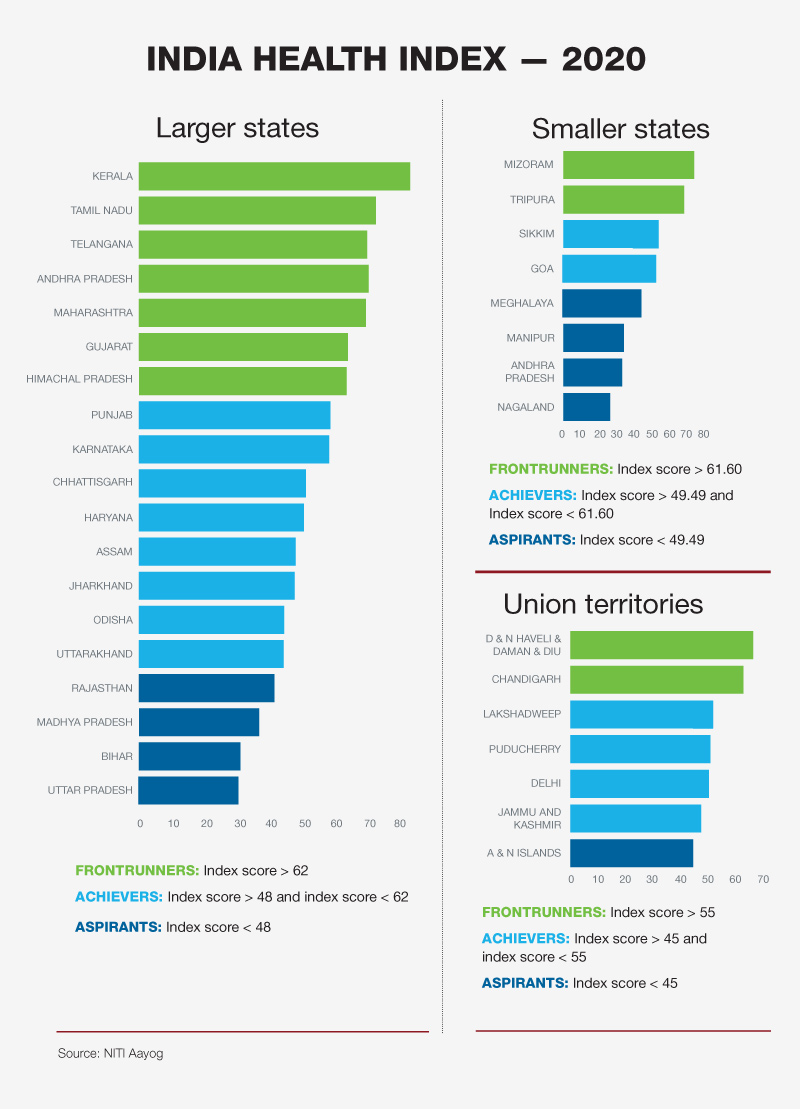
Considering the disparity in diseases and healthcare service delivery across the many states and union territories of the country, India can be described as many nations within a nation. The SDG India index 2020-21 for health shows Kerala, Tamil Nadu and Himachal Pradesh as frontrunners, while Bihar, Jharkhand, Assam and Uttar Pradesh continue to struggle.
Kerala and Tamil Nadu have achieved 99% institutionally delivered births. Kerala’s neonatal mortality rate is 6, which falls in the same bracket as the United States (4) and the United Kingdom (3). These two states, comparative laggards in economic growth, have emerged as leaders in public healthcare for three reasons: genuine universal healthcare access, innovations in frontline health delivery, and political will.
Improved facilities
Many of the frontrunners have implemented a multitude of state-level initiatives, resulting in improved access to healthcare facilities as well as strengthened healthcare systems. There are lessons to be learned here by those shuffling along far behind.
- Health issues should be tackled with an integrated approach that emphasises not just access to basic health services, but also to education, sanitation, food and clean water.
- The utilisation of government health centres improves when they are well staffed and well equipped. In the context, it is important for healthcare professionals to be given incentives for working in remote and underserved regions.
- The efficient administration of drugs and devices can result in the provision of superior healthcare services to the masses, thus reducing their out-of-pocket expenses. (Kerala and Tamil Nadu, again, score high on this count.)
- Ensuring decentralisation of health planning and programme implementation, down to the village level, leads to better health outcomes. This is a proven panacea.
- Political will plays a critical role in ensuring proper healthcare for all by prioritising public health, and by crafting innovative schemes to improve accessibility and affordability.