Not so rare, after all
Rare genetic diseases are debilitating for patients and their caregivers, but the situation is getting better as awareness and government support increases

Neeraja Chilukoti is a project scientist with the Centre for DNA Fingerprinting and Diagnostics, Hyderabad
Humankind has been battling diseases since time immemorial. Treatment protocols and the priority areas to tackle these diseases have been changing and improving due to the development of new therapeutic options. With the advent of vaccines and antibiotics, we have successfully eradicated many infectious diseases, and the focus has now shifted to noncommunicable diseases.
India is witnessing an increase in noncommunicable diseases, and genetic disorders form a major group of such medical disorders. To cite one example, congenital malformations are the fourth most common cause of mortality among newborns in urban parts of the country.

Ashwin Dalal is head of the diagnostics division at the Centre for DNA Fingerprinting and Diagnostics, Hyderabad
India is home to diverse cultures comprising different ethnic and linguistic groups. The Indian population is distinctly different from that of the rest of the world due to religious and cultural practices that encourage specific marriage patterns -- termed endogamy -- among communities. The practice of consanguinity, which includes marriage among close family members, is a tradition in many countries, and this leads to higher rates of genetic disorders.
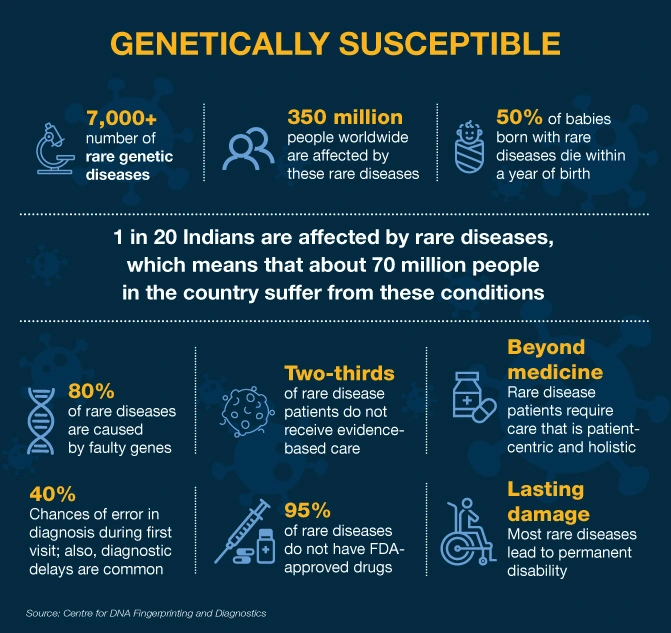
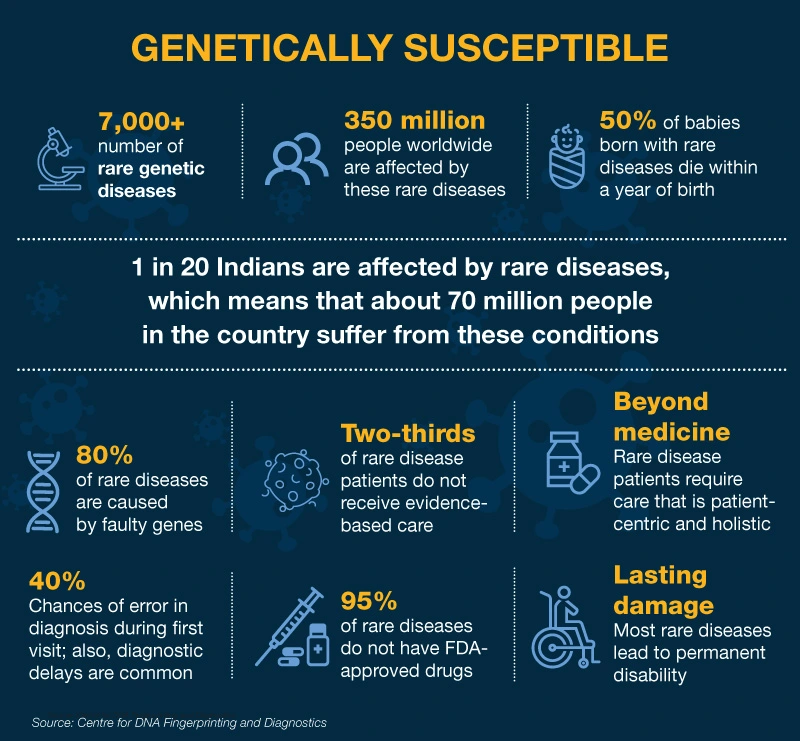
Rare diseases are debilitating and lifelong and they affect a small percentage of people. It is estimated that 80% of rare diseases are genetic in origin and they cause more damage to children. Rare genetic diseases (RGDs) pose a serious concern to public health in India because of our large population, which can translate to the rarest of rare diseases still being a huge burden. In India, it is estimated that 70 million people are affected by one of more than 7,000 classified RGDs.
Child fatalities
The commonly reported RGDs in India are haemophilia, thalassemia, sickle-cell anaemia, primary immunodeficiency, autoimmune diseases, lysosomal storage disorders and certain forms of muscular dystrophies. Of the RGDs, 50% of new cases are found in children — responsible for 35% of deaths before the age of one; 10% between the ages of one and five; and 12% in the five-to-fifteen age group. The landscape of Indian RGDs is dynamic and new rare diseases and conditions are being identified and reported regularly.
The first step to finding a solution to this problem is understanding the problem. India still does not have a definition for rare diseases due to the paucity of population-level data. A fundamental challenge in research and development to combat the majority of rare diseases is that relatively little is known about the pathophysiology or natural history of these diseases. Rare diseases are difficult to research as the patient pool is small, often resulting in inadequate clinical information.
The diagnosis of an RGD in a child is like a blow out of nowhere for a family. Parenting is extremely difficult for those with children suffering from life-threatening RGDs. Owing to limited awareness, parents end up approaching multiple hospitals, and the average duration taken for a final RGD diagnosis is about seven years. This diagnostic odyssey is only the beginning of hardships since the struggle to pay for treatment adds to the deteriorating financial and social condition of affected families.
Availability and access to medicines are important in reducing the morbidity and mortality associated with RGDs. Despite progress in recent years, effective and safe treatment is not available for most of these diseases. Although treatments are available for some RGDs, the cost is prohibitive and many medicines need to be imported. Hence, even when a correct diagnosis is made, there may not be an available therapy to treat the disease.
Less than 5% of rare diseases have therapies available to treat them. About 95% of rare diseases have no approved treatment and fewer than one in 10 patients receives disease-specific treatment. The Indian healthcare system is not yet geared to handle these patients and, in the absence of definitive treatments, patients have little to fall back on.
Activist parents
Some parents have turned into activists and have approached the government for a refinement of policies and to provide financial aid. It is their persistence and hard work that has led to RGDs coming to the notice of healthcare authorities. Despite all odds, these parents have continued to fight for the well-being of their children and pushed for government-backed programmes and policies to address the needs of those affected by RGDs.
RGDs being ‘rare’, many clinicians are not aware of the possibility of these conditions in their patients. There are encouraging signs, though. Genetic diagnostic facilities have increased considerably over the years, and they have become an integral part of healthcare delivery. These facilities are available now in different parts of the country and there is no need to send samples abroad for diagnostic testing, as was the case a few years ago.
With the advent of technologies such as microarray and next-generation sequencing, it is possible now to study the whole genome of an individual at a much more affordable cost. These technologies have revolutionised the field of genetic diagnostics.
Prevention of genetic disorders is the only way to decrease the burden of these diseases. Since most genetic diseases are not treatable, the only option is to prevent the birth of these children by prenatal diagnosis. Once the genetic abnormality is identified in the patient, prenatal diagnostic tests can be done in subsequent pregnancies to identify if the unborn foetus carries the same mutation.
Policy in place
The Indian government launched a ‘national policy for rare diseases’ (NPRD) in March 2021 for the overall management of RGD-affected patients. The salient features of the NPRD include policy recommendations on diagnosis, awareness, treatment and patient support. RGDs have been classified depending on the type of treatment needed and the cost of such treatment.
There is a provision in the NPRD to provide up to ![]() 5 million per patient to procure drugs for RGD treatment (this facility is provided through one of the 12 centres of excellence established under the policy). In addition, the policy promotes research and development for the diagnosis and treatment of RGDs, and pushes for the indigenous development and manufacture of affordable drugs.
5 million per patient to procure drugs for RGD treatment (this facility is provided through one of the 12 centres of excellence established under the policy). In addition, the policy promotes research and development for the diagnosis and treatment of RGDs, and pushes for the indigenous development and manufacture of affordable drugs.
Furthermore, the Department of Biotechnology, which is attached to the central government’s Ministry of Science and Technology, has launched a project called UMMID (Unique Methods of the Management and treatment of Inherited Disorders). This works on the concept of ‘prevention is better than cure’ and is a huge step forward to promote newborn and antenatal genetic screening in India.

The national sickle cell anaemia elimination programme, meanwhile, addresses the health challenges posed by sickle cell disease, particularly among tribal populations of the country. Additionally, the Department of Biotechnology has funded a pan-India project on paediatric rare genetic disorders with 16 collaborating centres. The project envisages an expanded programme for these disorders, spanning diagnostics, research and counselling.
In a nutshell, RGDs are a public health emergency that need to be addressed in a multipronged way, bringing together all stakeholders — including patients, parent support groups, media, healthcare services, diagnostic laboratories and pharmaceutical companies — so that India is better equipped to deal with these diseases and their fallout.