Eat right, start bright
The battle against child malnutrition and high-risk pregnancies has brought about a bunch of breakthroughs in Sirohi district
A rough map showing about 200 hut icons hangs on the wall of the anganwadi (childcare) centre in Nichlagarh village, about 70km from the district headquarter of Sirohi in south Rajasthan. Each icon represents a house in Nichlagarh and most of the houses are dotted with colourful bindis (a decorative dot worn in the middle of the forehead by Indian women): red, pink, yellow, blue and red-on-yellow. There’s a lot of red and yellow and that is a matter of concern.
The map and bindis are a nazri naksha (visual aid) that, at a glance, shows the health status of pregnant women and infants in the area. The blue bindis indicate homes with pregnant women, pink means homes with a new-born baby, red is for high-risk pregnancies and yellow for malnourished children. Red-on-yellow is a severely malnourished child, nine times more likely to die than a healthy child.
A preponderance of red and yellow implies women and babies at risk. In Nichlagarh’s 193 houses, there are two high-risk pregnancies and 37 malnourished children. The very fact that this data is available makes Nichlagarh a success story for the Tata Trusts and its nodal agency, Centre for microFinance (CmF), which works to improve maternal and child health as part of its health interventions in Sirohi.
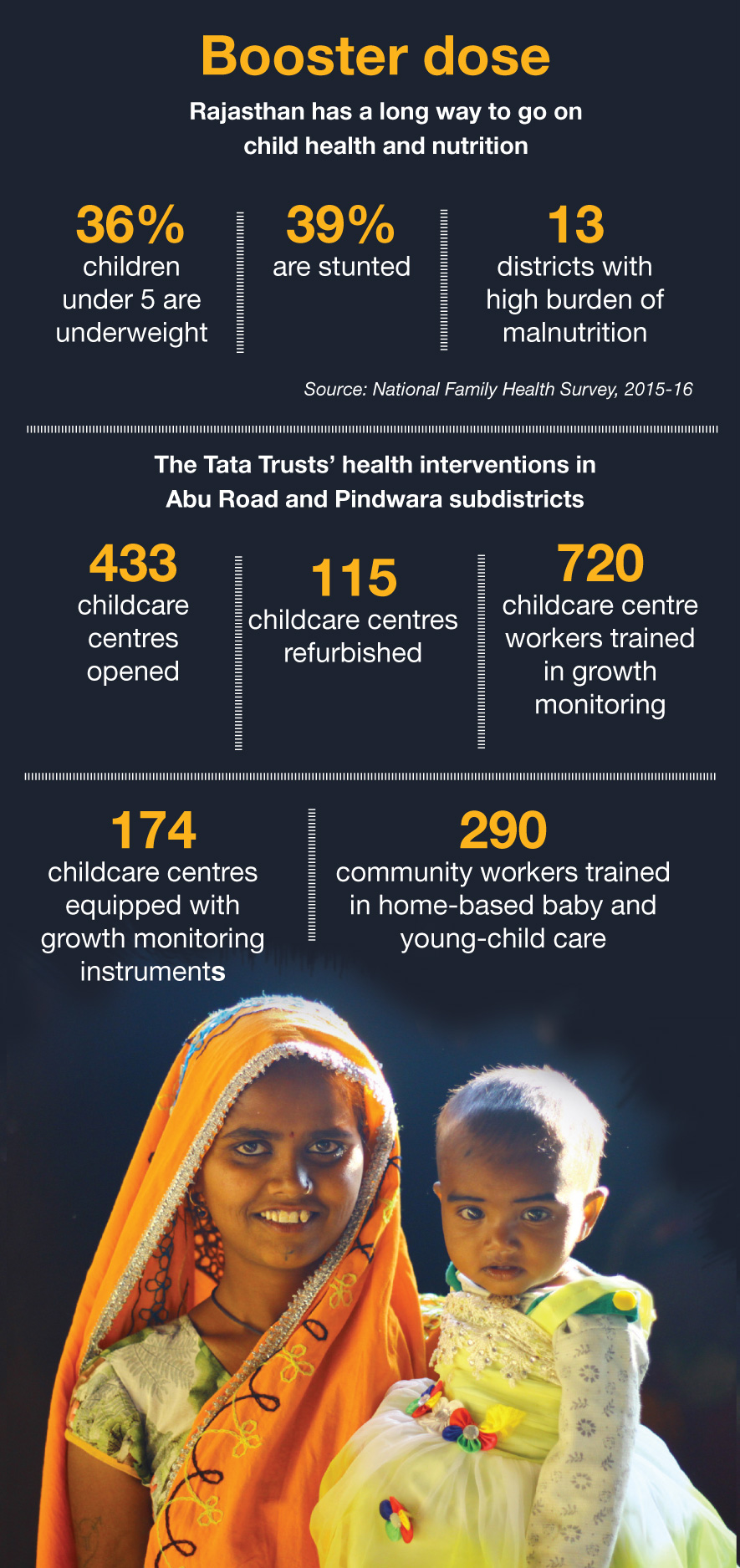
Rajasthan — and Sirohi in particular — has struggled with the battle against malnutrition. CmF is fighting to change this situation through a grassroots approach that focuses on processes and capacity building while monitoring the work of frontline workers.
At the village level, the responsibility of dealing with red and yellow cases rests on — not a doctor or a hospital — but on three women: the accredited social health activist (or ASHA), the auxiliary nurse midwife (ANM), and the anganwadi worker (AWW). Known as the AAAs, these women are the last-mile service providers of the government’s maternal and child health and nutrition (MCHN) programmes.
Mother, child and more
To keep women and babies healthy, the three need to work closely together. ASHAs go house-to-house to check on pregnant women and new mothers and babies. ANMs are responsible for providing pregnant women with antenatal health checkups, ensuring they get to a hospital for their delivery, and the immunisation of children. AWWs hand out the government-provided nutritional inputs (known as take-home rations) to the women and children.
Training, monitoring and supporting the AAAs have been at the core of CmF’s efforts to improve maternal and child health in Sirohi over the past four years. The biggest positive to emerge from the health intervention in the district came about because of a CmF survey of infants and children. Finding that nearly half the children in the villages surveyed showed signs of wasting and stunted growth, the survey brought the rampant malnutrition to the state government’s attention.
“We raised the issue at the subdistrict, district and state levels and they finally acknowledged the dire situation and requested our technical support in the field,” says Vijay Singh, general manager, CmF. “We realised that there was an alarmingly high incidence of malnutrition amongst the tribal population. CmF supported us in tackling this situation,” says Nitin Gehlot, the child development project officer for the Abu Road subdistrict under the government's integrated child development services (ICDS) programme.
To deal with the crisis, the government rolled out the Integrated Management of Acute Malnutrition (IMAM) project in 40 villages of Abu Road block. An intensive endeavour, it comprised a three-month exercise involving identification, treatment and checkups.

To identify malnourished children, the CmF team spread out with ASHA workers and screened some 8,600 children, measuring their mid-upper arm circumference (an indicator of malnutrition). Of these, some 1,450 children fell short on the required parameters and needed to be checked more thoroughly by ANMs.
A total of 400 children were identified to be severely malnourished. The government machinery responded by allocating energy-dense nutritional supplements for three months. The weight of the children was carefully monitored every week. Another 500 children, poised precariously on the borderline, were put on a regimen of double doses of the regular nutritional inputs. Twelve critical cases had to be sent to the Malnutrition Treatment Centre (MTC) at Sirohi for medical care.
Weighing it up
CmF also took on the onus of strengthening health systems and capacity building. A large part of the work involved training ANMs, AWWs and ASHA workers on the processes to be followed for weighing and measuring children, and documenting the data. Many anganwadi centres did not have weighing scales and stadiometers (to measure height), or even mats for the children to sit on. CmF extended the project plan to buy and install equipment where necessary.
Concerted efforts by CmF over the years have led to welcome outcomes. Today, more than 80% of the children less than five years old in Abu Road and Pindwara are being monitored regularly. The intensive exercise benefited many of the children but the challenge lies in changing the poor diets followed in the predominantly tribal households of the region.
This is why even after the three months of the IMAM project, over 130 children were still severely malnourished and had to be referred to the MTC. “Parents are not aware of what constitutes a healthy meal,” says Rakesh Panwar, CmF’s anchor for health and nutrition. The team is now working to change local food practices by organising community meetings on the importance of balanced diets using local foods.
CmF also supports the government’s efforts to organise poshan melas (nutrition fairs) to build community awareness on the link between food and health. The gram panchayat (village council) system has committees that are supposed to monitor health, water, sanitation and nutrition. CmF has trained members of 68 committees to effectively monitor health and nutrition services in their villages.
CmF’s health teams support ASHA and anganwadi workers in organising a MCHN day every month at anganwadis in Abu Road and Pindwara. On this fixed date, women and children come in and ASHA workers document the height and weight of every child.
Food traditions and poverty mean that the red and yellow bindis continue to mark the map. But the difference is that the government health system is now alert and active, and the tribal community is slowly waking up to the importance of nutrition.
The three ‘As’ score high
Meva Rata is 28 and has four children. For the fourth baby, she received the full complement of government health services: four antenatal checkups, institutional delivery and immunisation for the child. Unlike with her first three pregnancies, Ms Rata was on the ‘due list’ this time around.
The due list is maintained by Champa Bai, the accredited social health activist for Nichlagarh. Ms Champa visits every household to check whether any woman is pregnant and how mothers and babies are faring. She maintains a daily diary and carries around a kit for pregnancy tests, registration forms for pregnant women and contraceptives.
Every month, she shares the due list with Anusuya Angadi, the auxiliary nurse midwife for the area. Ms Angadi’s role is to monitor the health of women like Ms Rata. Regular blood tests, physical checkups and the monitoring of other parameters are part of the course. She also identifies high-risk pregnancies: women who are underweight, having their first baby or whose blood tests show a problem.
The high-risk cases are closely tracked by Ms Angadi and Ms Champa. When a baby is due, one of them will climb a slope to catch the mobile signal (because of its hilly terrain, Nichlagarh has poor network connectivity) and call 108, the government ambulance service.
When Ms Rata’s baby, Khusba, was born, the mother was counselled to only breastfeed and to maintain basic hygiene. Khusba was monitored regularly for the first 42 days of her life and has received all her vaccinations as per schedule. It’s Ms Champa’s duty to remind the mother and Ms Angadi’s to administer the shots.
Ms Rata and her baby get the regular rations of nutritional inputs at the anganwadi centre. Once Khusba is three years old, she will visit the centre for four hours a day. There she will get a freshly prepared hot meal, some fun activities to do, and the care of Nokhli Bai, the anganwadi worker.
Once a week, mothers, babies and children arrive at the anganwadi centre. Here, Ms Champa measures and documents the height and weight of every child in the neighbourhood. Malnutrition indicators are flagged and data recorded.
Ms Champa, Ms Angadi and Ms Nokhli are the fulcrum of the village health system that is at the core of Sirohi’s fight against malnutrition. These women bear a huge responsibility and they are the cadre of three ‘As’ that CmF trains and supports.